Cardiac Imaging for Preventive Care: Classifying Cardiovascular Risk and Promoting Longevity
- Dr Duy Dinh

- Aug 29
- 9 min read
Summary
Cardiac imaging is revolutionising preventive healthcare by enabling medical professionals to visualise the heart and blood vessels in remarkable detail, facilitating the early classification of cardiovascular risk. This patient-focused guide explores the main cardiac imaging modalities—echocardiography, cardiac computed tomography (CT), cardiac magnetic resonance imaging (MRI), and nuclear imaging—and explains how each supports risk stratification and the development of personal preventive health strategies. Understanding your individual cardiovascular risk empowers you to take targeted actions with your doctor, influencing not just your immediate health but long-term vitality and longevity. At Zelica Health, we use these advanced imaging tools, combined with telehealth expertise, to guide patients in taking the steps that matter most for heart health. Book a preventive care appointment or subscribe to our health programs today to be proactive about your future.
Table of content
What Is Cardiac Imaging in Preventive Care?
Why Classifying Your Cardiovascular Risk Is Essential
Cardiac Imaging Modalities in Preventive Care
Echocardiography: The Ultrasound Window to Your Heart
Cardiac Computed Tomography (CTCA and Calcium Scoring)
Cardiac Magnetic Resonance Imaging (MRI)
Harnessing Cardiac Imaging for Personalized Preventive Strategies
The Impact of Early Detection on Health Outcomes
Longevity Strategies: Preventive Health and Your Heart
Zelica Health: Telehealth Preventive Cardiology for the Modern Age
Taking Action: Book Your Cardiac Risk Assessment With Zelica Health

What Is Cardiac Imaging in Preventive Care?
Cardiac imaging refers to a set of non-invasive and minimally invasive techniques used to visualize the heart’s structure and function and assess the health of coronary blood vessels. The goal of preventive cardiac imaging is not just to diagnose existing symptoms, but to catch subtle abnormalities and risk factors before they evolve into serious heart conditions. Early detection through imaging allows for the classification of individuals into low, intermediate, or high cardiovascular risk categories and helps design tailored interventions that prevent the development or progression of heart disease.
Why is this important?Because cardiovascular diseases—including heart attacks, strokes, and heart failure—remain the world’s leading cause of illness and premature death, and many of these events can be prevented with timely identification of risk and intervention. Cardiac imaging acts as the doctor’s window into the heart, providing actionable data long before symptoms appear.
Why Classifying Your Cardiovascular Risk Is Essential
The Benefits of Knowing Your Risk
The identification and classification of cardiovascular risk are fundamental pillars of preventive healthcare. Patients who understand their risk profile can make informed decisions with their doctors about lifestyle modifications, medications, and the need for more frequent or targeted screenings. Key benefits include:
Early detection of disease when it is most treatable.
Personalized preventive strategies—no “one size fits all.”
Optimal allocation of healthcare resources—targeting those at greatest risk.
Improved outcomes and reduced need for invasive interventions.
Greater patient engagement and empowerment—motivating lifelong health changes.
Risk classification, using both traditional assessment tools (like blood pressure, cholesterol, diabetes, and family history) and modern imaging-based biomarkers (such as coronary calcium scoring and plaque characterization), allows a tailored approach to prevention and higher rates of success.
Classification Systems for Cardiovascular Risk
Globally and in Australia, the Framingham Risk Score and the ASCVD calculator are widely used to estimate 10-year risk of a heart attack or stroke. These calculators integrate:
Age and sex
Systolic blood pressure
Cholesterol (total and HDL)
Smoking status
Diabetes history
Family history of cardiovascular disease
However, many patients are not identified as high risk before a problem arises, hence the value of supplementing these tools with imaging-based measures.
Cardiac Imaging Modalities in Preventive Care
Below, we detail the main imaging options that help stratify cardiovascular risk—focusing on their role in preventive medicine, patient experience, and the actionable insights they provide.
Table: At-a-Glance—Main Cardiac Imaging Modalities for Preventive Care
Imaging Modality | What It Shows | Common Preventive Indications | Patient Experience |
Echocardiography (Echo) | Heart structure, function, blood flow, valve disease | Hypertension, murmurs, heart failure risk | Non-invasive, painless |
Cardiac CT (CTCA, CAC) | Coronary artery blockages, calcium burden, vessel anatomy | Coronary artery disease, risk stratification | Brief, low-dose X-ray |
Cardiac MRI | Tissue damage, fibrosis, functional assessment | Cardiomyopathy, myocarditis, early damage | Non-invasive, radiation-free |
Nuclear Imaging (SPECT/PET) | Blood flow/perfusion, tissue viability | Ischemia, coronary artery disease, viability | Injection, light radiation |
Each of these modalities plays a unique yet often complementary role in preventive cardiology.
Echocardiography: The Ultrasound Window to Your Heart
Echocardiography (including transthoracic, transesophageal, and stress echo) uses ultrasound waves to produce detailed live images of your heart’s chambers, muscle thickness, valves, and blood flow patterns. It is considered the first-line imaging tool for preventive cardiology because it is widely available, non-invasive, and free of radiation.

What it can reveal:
Underlying or early left ventricular hypertrophy (a sign of chronic hypertension)
Heart valve disorders that increase stroke risk
Early heart failure or reduced ejection fraction, even before symptoms
Cardiomyopathy detection, including hereditary or subclinical cases
Major strengths for preventive care:
Detects silent structural changes before symptoms emerge
Guides lifestyle and medication interventions
Monitors disease progression or improvement over time
Many major heart conditions are first detected via echocardiograms during routine screenings or targeted preventive visits. Regular echoes can be particularly important if you have high blood pressure, a family history of heart disease, or a detected cardiac murmur.
Cardiac Computed Tomography (CTCA and Calcium Scoring)
Cardiac CT includes two powerful tools in preventive care:
Coronary Artery Calcium (CAC) Scoring: This simple, low-radiation scan measures calcified plaque in the coronary arteries—an independent, highly specific marker of atherosclerosis and a strong predictor of future coronary events.
Coronary CT Angiography (CTCA): Visualizes the coronary arteries in detail, revealing both calcified and non-calcified plaques, and can detect blockages long before a heart attack strikes.

Benefits of Cardiac CT Imaging:
CAC scoring is non-invasive, takes only minutes, and involves no injection—making it ideal for risk assessment in asymptomatic individuals.
CAC is best suited for those with intermediate risk (not too low or high) based on clinical calculators, but can be considered earlier in those with a strong family history or diabetes.
CTCA has very high accuracy for ruling out coronary artery disease, reducing the need for invasive angiograms.
A CAC score of zero is a powerful negative risk factor—patients have an excellent prognosis and may avoid unnecessary medication unless other risks are present. Conversely, higher scores indicate the need for aggressive risk management, with statin and/or aspirin therapy as appropriate.
Cardiac Magnetic Resonance Imaging (MRI)
Cardiac MRI uses magnetism and radio waves (not X-rays) to create highly detailed images of the heart’s tissues and function. It is the gold standard for detecting subtle tissue changes or early damage, especially in:
Cardiomyopathies (heart muscle diseases, often inherited)
Myocarditis (inflammation), fibrosis (scarring), or infiltration
Valvular abnormalities and congenital heart disease
Silent post-heart attack damage
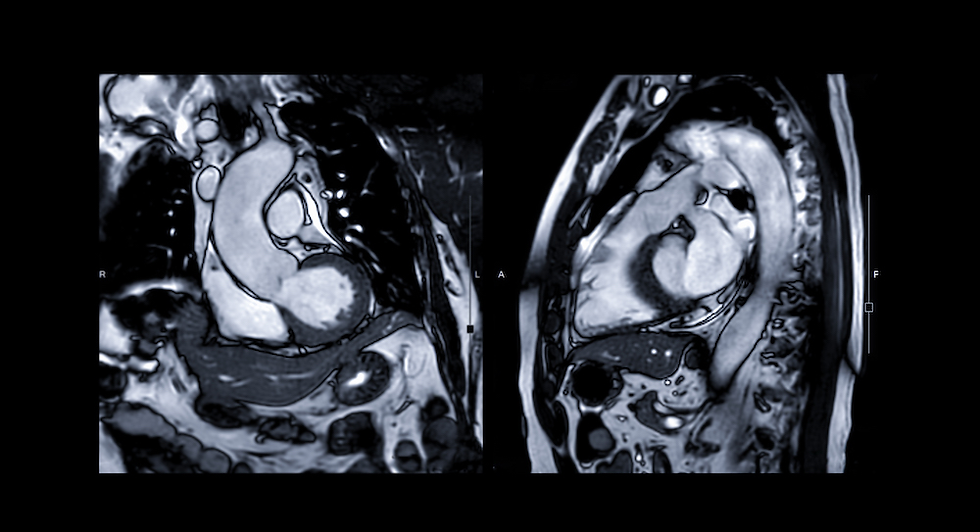
Preventive strengths of MRI:
Identifies silent, early-stage disease and areas at risk of arrhythmia
Provides prognostic information that may guide whether intensive preventive therapy is indicated in the absence of conventional symptoms
Can be crucial for those with a family history of sudden cardiac death, unexplained symptoms, or poorly visualized hearts on other imaging
MRI is rapidly advancing with artificial intelligence tools that further refine risk classification and prediction, potentially before any symptoms or routine blood markers are abnormal.
Nuclear Imaging (SPECT, PET)
Nuclear imaging involves injecting a small amount of safe radioactive tracer to visualize blood flow through your heart’s tissues, often during rest and stress.
SPECT (Single-Photon Emission Computed Tomography) measures blood flow and identifies areas of reduced perfusion under stress—all valuable for detecting “hidden” blockages or early disease.
PET (Positron Emission Tomography) provides even more sensitive images, sometimes highlighting microvascular dysfunction—impaired blood flow before any anatomical plaque is visible.

Why nuclear imaging matters for prevention:
Confirms or excludes ischemia (lack of blood supply) in patients with risk factors or atypical symptoms.
Predicts risk of future events—a completely normal scan is associated with very low risk for several years.
Guides decisions on whether further imaging or invasive therapy is needed.
While not typically first-line for routine risk screening, nuclear methods are often the next step after equivocal or high-risk findings on echo or CT.
Harnessing Cardiac Imaging for Personalized Preventive Strategies
Cardiac imaging does more than screen for disease; it creates an individualized picture—your heart’s own biography. By integrating imaging results with traditional risk scores (like Framingham or ASCVD), a doctor can stratify your risk with far greater precision and tailor preventive recommendations. This is the essence of personalized medicine.
For example:
A person with intermediate clinical risk but zero calcium score may confidently avoid lifelong medication.
An individual with mild symptoms but a high plaque burden on CTCA may start preventive therapy early—potentially averting a heart attack.
A family history of sudden cardiac death, with early abnormality on MRI or echo, can trigger advanced prevention (lifestyle, medication, or monitoring for arrhythmias).
This precision approach enhances both effectiveness and cost-efficiency, prioritizing treatment for those who need it most while reassuring and safely monitoring others.

The Impact of Early Detection on Health Outcomes
Why Early Heart Risk Detection Is Life-Changing
Early detection of cardiovascular risk and subclinical disease is consistently associated with better long-term health outcomes:
It enables timely action—lifestyle modifications, medication, or further evaluation—before irreversible damage sets in.
Patients managed earlier often avoid or delay major cardiac events, reducing hospitalization and healthcare costs.
Many studies reveal that early coronary calcium screening and advanced imaging in intermediate-risk patients can reclassify risk and directly reduce unnecessary treatment or missed opportunities for prevention.
A normal imaging result provides substantial reassurance and often helps “de-medicalize” healthy people, allowing better focus of resources. On the flip side, identifying silent high-risk patterns motivates adherence to treatments and lifestyle changes, as patients “see” the early impact of risk factors on their own heart.
Real-World Outcomes: The Evidence
Patients with zero calcium score demonstrate <1% risk of heart attacks or stroke over a decade, frequently avoiding medication unless new risk factors arise.
Imaging-guided preventive care leads to lower rates of invasive angiography, heart attacks, and sudden deaths, according to large multicenter studies.
Patients with early detection of silent cardiomyopathy or heart failure managed in the community live longer, with less disability, compared to those diagnosed only after a hospitalization.
In short, getting your cardiac risk classified early empowers you to act and live better, for longer.

Longevity Strategies: Preventive Health and Your Heart
Evidence-Backed Actions for a Long, Heart-Healthy Life
Longevity in today’s world hinges not just on medical technology, but on proactive action based on your unique risks and needs. Major research has established that people who keep their “Life’s Essential 8” (healthy blood pressure, cholesterol, blood sugar, weight, sleep, diet, activity, and no tobacco) in check live longer—with quality of life and fewer chronic illnesses.
However, many silent heart risks go undetected for years, even with normal checkups. This is why combining lifestyle vigilance with strategic, personalized cardiac imaging is so powerful:
It translates invisible risk into actionable insights for you and your doctor.
Motivates and monitors progress on the “big 8.”
Guides which medications, supplements, or therapies fit your risk window.
Identifies and corrects treatable causes, like silent valve disease or inherited heart conditions.
Preventive Actions You Can Take—With Medical Partnership
Schedule a risk assessment: Ask about your blood pressure, cholesterol, glucose, and if eligible, a calcium score or echocardiogram.
Partner with a doctor or clinic specializing in preventive and longevity care—like Zelica Health—so your care is guided by both test results and the latest global evidence.
Don’t “wait for symptoms”—most people who have a heart attack never experience warning signs.
Discuss your family history and ask what imaging might be most valuable for your particular profile.
Make sustainable lifestyle changes, using imaging results as visual feedback to stay motivated.
Remember: Prevention is not one-and-done. It’s an ongoing collaboration—checking in, re-measuring, and adjusting as you age.
Zelica Health: Telehealth Preventive Cardiology for the Modern Age
Why Choose a Telehealth Preventive Heart Clinic?
With the rise of telehealth, comprehensive preventive cardiology is now accessible to everyone—regardless of location or schedule. At Zelica Health, our mission is to deliver advanced, personalized preventive care and expert medical advice, online and on your terms:
General and risk assessment appointments: Get your profile reviewed by an AHPRA-registered doctor without travel or waiting.
Health subscription programs: Sign up for regular, structured check-ins, monitoring, and adjustment of your preventive plan.
Personalized prevention plans: Combine traditional risk scores, imaging, genetics, and biomarkers for your own life-optimization strategy.
Long-term follow-up and proactive health coaching, covering cardiac risk as well as metabolic, cancer, and longevity factors.
Accessible from anywhere in Australia, supporting all ages and backgrounds with compassion and expertise.
We believe that “why wait for disease when you can prevent?”—and that empowering patients with information and an actionable, realistic plan is the best investment in lifelong health.
Taking Action: Book Your Cardiac Risk Assessment With Zelica
Why You Should Act Now
Your heart’s future is in your hands. Cardiac imaging for preventive care is your invitation to understand your individual cardiovascular risk—and take evidence-based steps, guided by a medical professional, to improve your odds of long, healthy living.
Whether you want to book a one-off heart checkup or join a subscription program for ongoing personalized preventive care and health optimization, Zelica Health is here to help you every step of the way with telehealth convenience and clinical excellence.
Don’t wait for symptoms—be proactive:
Book your preventive heart appointment or subscribe to a personalized health program at Zelica Health today. Start investing in your longevity!
📚 References
Kashyap, M., Ansari, T., Kumari, A., Kumari, S., & Kumar, C. (2025). Imaging Modalities in Assessing Cardiovascular Risk Factors. International Journal of Research and Technology Innovations, 5(7), Article IJRTI2507101. Retrieved from https://ijrti.org/papers/IJRTI2507101.pdf
Nixdorff, U., Achenbach, S., Bengel, F., Faggiano, P., Fernández, S., Heiss, C., Mengden, T., Mureddu, G. F., Nagel, E., & Puntmann, V. (2015). Imaging in Cardiovascular Prevention. In The ESC Textbook of Preventive Cardiology (pp. 54–76). Oxford University Press. https://doi.org/10.1093/med/9780199656653.003.0006
European Society of Cardiology (ESC), European Association of Cardiovascular Imaging (EACVI). (2023). Consensus and Position Papers on Cardiovascular Imaging. Retrieved from https://www.escardio.org/Guidelines/Scientific-Documents/Recommendations-and-position-papers
MDPI Editorial Team. (2023). Role of Cardiovascular Imaging in Risk Assessment: Recent Advances. Journal of Clinical Medicine, 12(17), Article 5563. Retrieved from https://www.mdpi.com/2077-0383/12/17/5563
Australian Prescriber. (2023). The Role of Cardiac Imaging in Clinical Practice. Retrieved from https://australianprescriber.tg.org.au/articles/the-role-of-cardiac-imaging-in-clinical-practice.html



Comments